According to the Centers for Disease Control, a multidrug-resistant fungus, Candida auris, is beginning to spread in numerous countries, including the United States where a total of 617 cases have already been reported. Of these cases, 309 have been reported in New York, while Illinois and New Jersey have also reported high numbers and more cases are currently present in nine other states. However, this is not the first time the C. Auris fungus has emerged. Symptoms might not be noticeable because patients infected with C. auris are often already sick in the hospital with another serious illness or condition. The symptoms of C. auris infection depend on the body part that is affected. For bloodstream infections, the most common symptoms are fever and chills.
The very first case of the C. auris fungus was discovered in 2009, upon testing of the ear discharge of a patient in Japan. At the time, there were very few reports of the fungus, however throughout 2018 and 2019 such reports are on the rise. Currently, cases of C. auris have also been reported in South America, South Africa, and Asia. It is likely that the fungus was introduced to the United States when a patient or multiple patients received healthcare from an area where the pathogen has already spread and then returned to the United States.
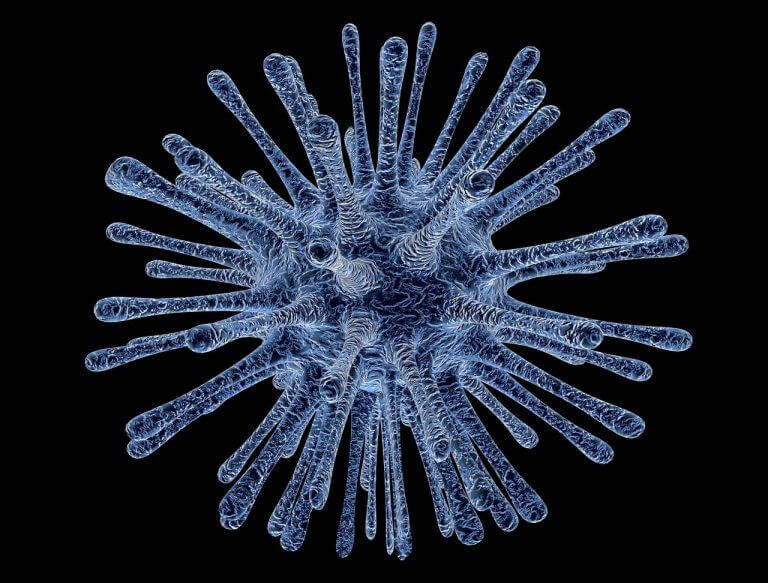
But, what exactly is the fungus and how dangerous is it? One of the major concerns of the C. auris fungus is that it is difficult to diagnose and seemingly impossible to treat given its resistance to multiple antibiotics. This resilient fungus can be spread through contact with a person exposed with fungus or even through objects where the pathogen has colonized. Patients infected with C. auris have been reported to suffer from severe bloodstream and wound infections, as well as ear infections.
According to the CDC, the risk of contracting this fungus is fairly low for the average household. However, individuals that have received treatment from a hospital where the pathogen has been reported, as well as individuals who have used antibiotic and antifungal prescriptions extensively, are at a much higher risk. The risk is also higher for patients who have recently undergone surgery and for those with diabetes.
Upon diagnosis of C. auris, determining a treatment plan is difficult. Unlike other common fungal infections, C. auris is resistant to numerous types of antibiotics and antifungals. Given the consequences this pathogen can have, worry has grown that C. auris could add to the number of deaths caused each year due to drug-resistant pathogens. While C. auris is technically a fungus, its resiliency to cooler temperatures, which allow it to easily colonize on the skin’s surface, more closely mimics the behavior of bacteria.
It is estimated that at least 23,000 people die in the United States each year as a result of contracting an antibiotic-resistant infection, and globally these numbers are much higher. However, as C. auris remains resistant to available treatments and continues to spread, it seems those numbers may soon be on the rise.
To learn more about cases like this or to access numerous resources on different types of fraud, visit the Jeff Newman Law Whistleblower Help Center and blog!